By: Javacia Harris Bowser
Your zip code shouldn’t determine how healthy you are. Unfortunately, we live in a society where it often does. But Albert Schweitzer Fellow Chelsea Gayre is doing her part to try to help change that.
For her Fellowship project, Chelsea teamed up with Bullock County Hospital, Vital Engine LLC, and Dr. Stephen Clarkson of the University of Alabama at Birmingham to provide specialty care consultations for primary care patients in Union Springs, Alabama using a telemedicine platform.
“The project was derived out of an interest for specialty care with cardiology,” says Chelsea, who has a background in cardiac nursing and is currently pursuing a family nurse practitioner degree at Auburn University’s College of Nursing. “But the more we started researching into the background, the demographics, what the area actually had, and where it lies within the state, we found that there’s actually this huge disparity in services in general.”
Bullock County faces a patient to physician ratio of 3379 to 1 for primary care services. The residents in the area have high incidences of diabetes and hypertension as well as heart disease.
“They also have a large population of Medicaid recipients,” Chelsea adds. “The average age is age 39 – so it’s a very young, uninsured population with health disparities.”

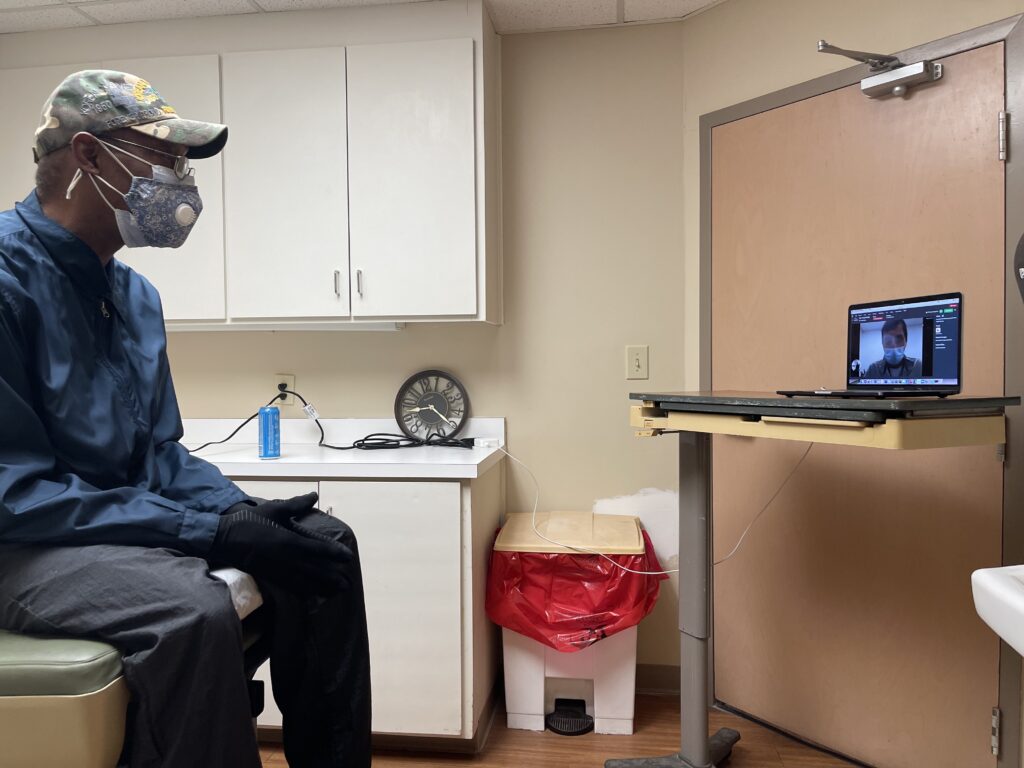
Using telemedicine to address health disparities in rural communities is challenging because patients may not have access to internet services needed for video chats. So, Chelsea got creative. For her project’s patients who needed cardiac health services, they received a referral from their primary care physician and then returned to the health care facility to have a telemedicine visit with Dr. Stephen Clarkson of UAB using a platform provided by Vital Engine LLC.
“I felt this project was important for a few reasons,” Dr. Clarkson says. “First, cardiovascular disease still remains the leading cause of death among Americans and rural communities are facing higher overall mortality. This mortality gap is widening, even in spite of the medical advancements to treat cardiovascular disease. Second, a major problem facing individuals living in rural communities is access to care.”
Dr. Clarkson went on to explain that studies show limited specialist coverage in rural communities is associated with differences in mortality.
“When you combine worsening mortality with lessening coverage, this creates a public health problem,” he says. “Chelsea’s project seeks to identify a creative solution for this pending public health problem by utilizing established healthcare infrastructure (from primarily urban centers) to remotely provide access to those living in rural communities. This is the first step into understanding what resources are needed to provide access to safe, equitable, and effective care to those living in rural communities, thereby reducing disparate cardiovascular disease morbidity and mortality.”
Chelsea was on site to take vitals, answer questions, and troubleshoot any technological issues that may have arisen. She also used the opportunity to stress the importance of primary care. Chelsea would also talk to patients to determine their satisfaction with their health care and she always asked if all of their health concerns had been addressed during a visit.
“Everybody had a very unique story,” Chelsea says of the patients she had an opportunity to work with during her project. “A couple of them said they had been referred out before and they had actually seen other cardiologists, but they had to travel. There was nothing closer than an hour for them to get to a specialist, and then they would get there, and they would feel like nothing was individualized for them. ‘They didn’t have enough time to spend time with me,’ they said. And so, the fact that we were there, and we had an interest in them and we were trying to listen to them and what they felt like they needed for their health care, meant a lot. It was touching.”
For Chelsea, this project is personal.
“I am originally from a very small rural community,” says the Carrollton, Ohio native.
“I grew up on a dairy farm and we had one primary care in the entire county very similar to Bullock. I have firsthand seen what it’s like for people not to get health care and have very low education about why they should get health care. So, I felt like this was a good chance for me to give back.”